October 2017
By Dr. Margaret Smith, GPO, BC Cancer Agency Vancouver Island Centre
Canadian Cancer Statistics 2016
Analysis by: Health Statistics Division, Statistics Canada
Data source: Canadian Cancer Registry database at Statistics Canada
In the general population of BC, Human Papilloma Virus (HPV) is pervasive. There is an estimated 80% risk of mucocutaneous infection in all Canadians by the time they reach age 50. Humans are the only reservoir for this double stranded DNA virus. Most infections are transient and are cleared by the host within 6 to 12 months, making the true incidence of HPV infection difficult to determine. There is increasing evidence that HPV can enter a latent state, with the potential to reactivate later in life and in immunocompromised hosts. Re-infection is possible by the same or different strain of HPV and is not uncommon.
Of the more than 40 HPV types known, the oncogenic strains are 16, 18, 31, 33, 45, 52 and 58, with strains 16 and 18 representing the bulk (70%) of HPV related cancer cases worldwide. Strains 6 and 11 are a common cause of anogenital warts. These nine strains are the components of the nonavalent HPV vaccine. The oncogenic strains have tropism or predilection to infect the rapidly dividing immature cells of squamocolumnar transformation zones, particularly the cervix, the anus, and the deep crypts of the tonsils. These are areas where HPV infection is more likely to persist, and with time cause cancer of the cervix, the anus, and the posterior oropharynx , including tonsil and base of tongue. Oncogenic strain HPV infection is on the rise in the younger generation during their first 10 years of sexual activity, and in the 50 plus age group. The time from initial oncogenic HPV infection to development of carcinoma in situ is generally 10 years, but can occur more rapidly in some individuals.
The host immune system is known to play an important factor in the natural history of HPV, as the incidence of HPV related cancers are greatly increased in patients with HIV/AIDS and following solid organ transplant. In population studies, HPV vaccination seems to give a more durable host immune response than natural infection does. It has also been observed that women treated for precancerous cervical lesions seem to benefit from subsequent HPV vaccination, when compared to those who do not receive vaccination following treatment. The mechanism is unknown, but may relate to subsequent re-infection with the same or a different oncogenic strain, or reactivation of a latent infection.
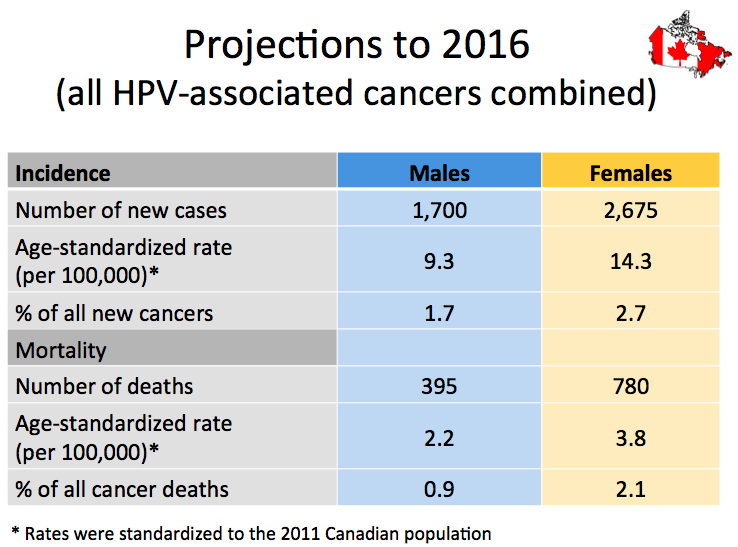
Canadian Cancer Statistics 2016 show there were 3,760 new cases of HPV related cancers in 2012, 64% female and 36% male.
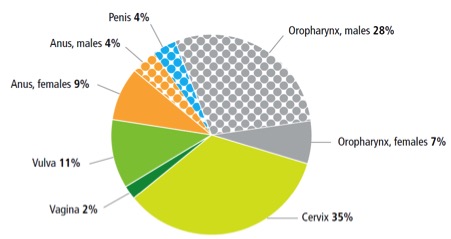
- Oropharyngeal and cervical are the most common areas of involvement, followed by anal and vulvar cancers;
- Cervical cancer incidence significantly decreased following the introduction of screening programs, but has been stable since 2005;
- HPV related anal cancer is increasing by 3.1% per year (3.3% in females, 2.2% in males);
- Vulvar cancer is increasing by 1.7 % per year; and
- HPV related oropharyngeal cancer is rising by 3.1 % per year in males and 1.1 % per year in females, and in men is poised to surpass the rate of cervical cancer in females in the near future.
This is the tip of a very large iceberg. Some cancers of the penis and vagina are HPV related, particularly in younger patients; however, these are still relatively uncommon. Oropharyngeal and anal cancers are difficult to detect early, and have often spread to regional lymph nodes by the time of diagnosis. The answer lies in prevention, and vaccination of both males and females is strongly indicated to reduce the incidence of HPV associated malignancies, as well as to provide a herd immunity effect. The tools to do this are available now! See related article in CMAJ Aug 14, 2017: http://www.cmaj.ca/content/189/32/E1030.full
Contact Dr. Margaret Smith: msmith@bccancer.bc.ca